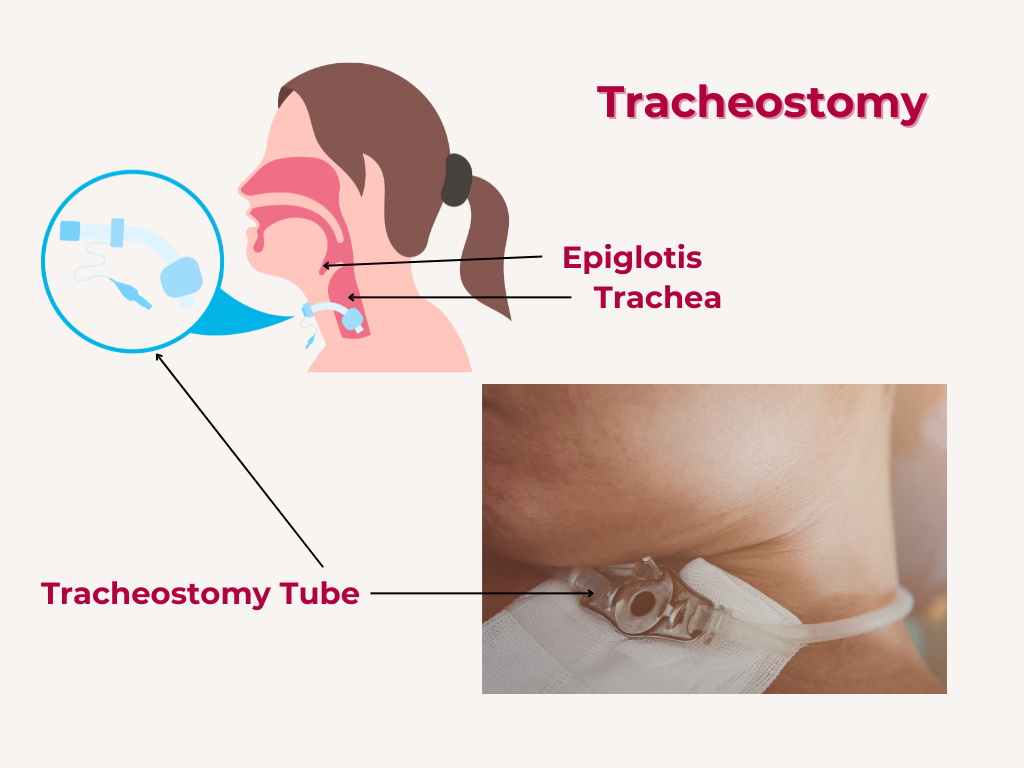
Tracheostomy is a surgical procedure that creates an airway by making an incision in the trachea to communicate with the skin and inserting a tube into the opening.
It has a long history dating back to ancient civilizations, with evidence of tracheostomy-like procedures found in Egyptian and Greek medical texts.
Anatomy and Site
1. Trachea: The trachea is a tube that extends from the larynx to the bronchi.
2. Site for tracheostomy: The ideal site for tracheostomy is between the 2nd and 3rd tracheal rings.
Types of Tracheostomy
1. High tracheostomy: Above the 1st tracheal ring
2. Mid tracheostomy: Between the 2nd and 3rd tracheal rings.
3. Low tracheostomy: Below the 3rd tracheal ring.
Indications
Upper airway obstruction
Tracheostomy may be indicated for upper airway obstruction due to various causes.
Causes of upper airway obstruction
Here are the causes of Upper Airway Obstruction (UAO), categorized by congenital and acquired causes
Congenital Causes
-
1. Choanal atresia:
A congenital condition where the nasal passages are blocked.
-
2. Laryngomalacia:
A condition where the soft tissues of the larynx are floppy, causing partial airway obstruction.
-
3. Tracheomalacia:
A condition where the tracheal cartilage is soft and floppy, causing airway obstruction.
-
4. Subglottic stenosis:
A narrowing of the airway below the vocal cords.
Traumatic Causes
-
1. Facial trauma:
Trauma to the face or neck can cause upper airway obstruction.
-
2. Laryngeal trauma:
Direct injury to the larynx can cause obstruction.
-
3. Iatrogenic trauma
Trauma during head and neck surgery
Inflammatory Causes
-
1. Epiglottitis:
Inflammation of the epiglottis, often caused by infection.
-
2. Laryngitis:
Inflammation of the larynx, often caused by infection or irritation.
Infective Causes
-
1. Croup:
A viral infection that causes inflammation of the larynx and trachea.
-
2. Diphtheria:
A bacterial infection that can cause a membrane to form over the tonsils and airway.
-
3. Retropharyngeal abscess :
severe retropharyngeal abscess can cause airway obstruction requiring tracheostomy and incision and drainage: refer case write up on retropharyngeal in groove health com
Neoplastic Causes
Benign
-
1. Laryngeal papillomas:
Benign tumors that can grow in the larynx.
-
2. Hemangiomas:
Benign tumors that can occur in the airway.
Malignant
-
1. Laryngeal cancer:
Cancer of the larynx.
-
2. Oropharyngeal cancer:
Cancer of the oropharynx.
-
3. Hypopharyngeal
carcinoma - advanced.
-
4. Nasopharyngal
carcinoma - advanced
-
5. Non - Hodgkin's
lymphoma with airway compromise
Neurological Causes
-
1. Vocal cord paralysis:
Weakness or paralysis of the vocal cords from tumours, surgery, neck injuries from accidental or assault .
-
2. Neuromuscular disorders:
Certain neuromuscular disorders can cause upper airway obstruction.
Miscellaneous Causes
-
1. Foreign body aspiration:
Inhalation of a foreign object into the airway.
-
2. Angioedema:
Swelling of the airway tissues, often caused by allergic reactions.
-
3. Obstructive sleep apnea:
Repeated episodes of upper airway obstruction during sleep.
Prolonged ventilation
Tracheostomy may be indicated for patients requiring prolonged mechanical ventilation.
Prolonged endotracheal intubation refers to the extended use of an endotracheal tube (ETT) to support a patient's breathing. The duration considered "prolonged" can vary depending on the context and patient population.
General Guidelines
-
1. Adults:
Intubation for more than 7-14 days is often considered prolonged.
-
2. Children:
The duration considered prolonged may be shorter, often around 3-7 days.
Risks Associated with Prolonged Intubation
-
1. Laryngeal and tracheal injury:
Prolonged pressure on the larynx and trachea can cause injury, including ulceration, granulation tissue formation, and stenosis.
-
2. Vocal cord damage:
Prolonged intubation can cause vocal cord paralysis or weakness.
-
3. Increased risk of ventilator-associated pneumonia (VAP):
Prolonged intubation increases the risk of developing VAP.
Prolonged endotracheal intubation may lead to consideration of tracheostomy, which can provide a more stable and secure airway, reduce the risk of laryngeal and tracheal injury, and improve patient comfort.
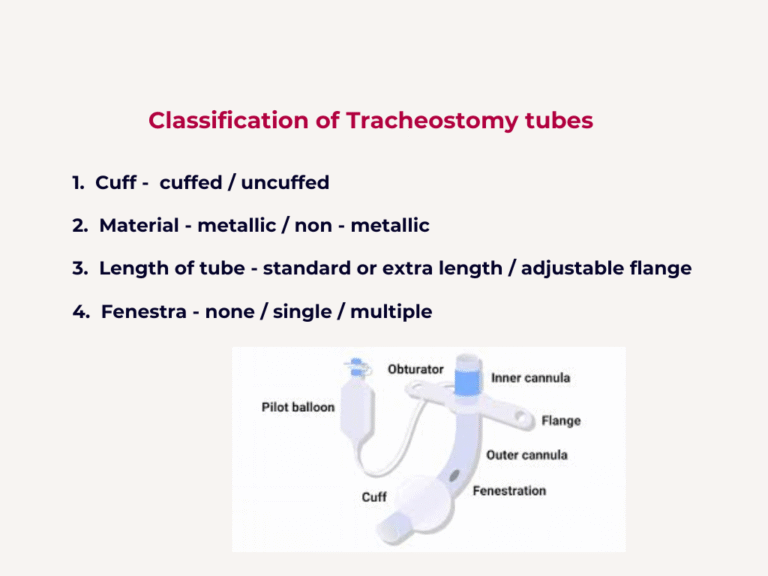
Tracheostomy Tubes
Types of Tubes
-
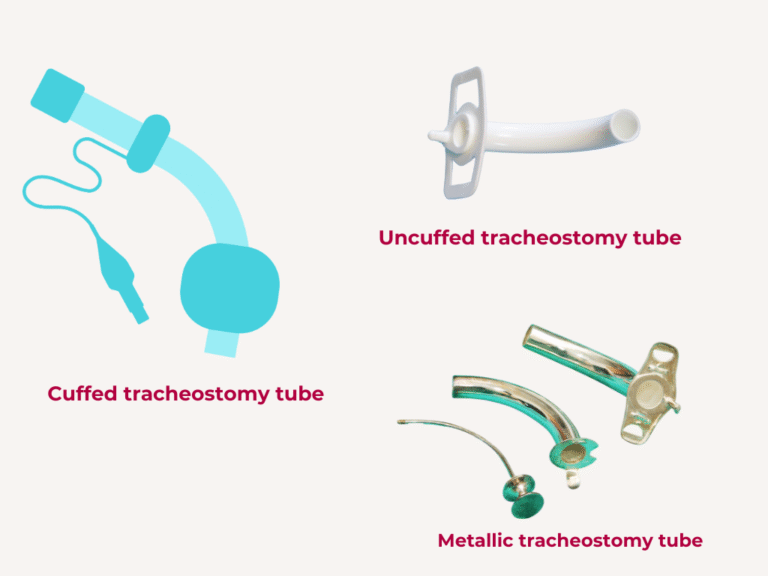
1. Cuffed and uncuffed tubes:
Cuffed tubes have an inflatable cuff to prevent aspiration.
-
2. Single cannula and double cannula tubes:
Double cannula tubes have an inner and outer cannula.
-
3. Fenestrated and unfenestrated tubes:
Fenestrated tubes have holes to allow airflow through the upper airway.
Selection of Tracheostomy Tube Size
The size of the tracheostomy tube in adult is selected based on the patient’s anatomy and the intended use. For children, the size of the tracheostomy tube may be selected based on the child’s age and size.
There isn’t a single, universally accepted formula for calculating tracheostomy tube internal diameter (ID) using age and weight.
However, some general guidelines and formulas are used:
Age-Based Guidelines
1. Newborns (0-1 month): 3.0 – 3.5 mm ID
2. Infants (1-12 months): 3.5 – 4.5 mm ID
3. Toddlers (1-3 years): 4.5 – 5.5 mm ID
4. Children (4-10 years): 5.5 – 7.0 mm ID.
Clinical Judgment
Ultimately, the selection of tracheostomy tube size should be based on clinical judgment, taking into account the individual patient’s anatomy, respiratory needs, and medical condition.
It’s essential to consult with experienced healthcare professionals and follow established guidelines and protocols when selecting tracheostomy tube sizes for patients.
Sizing Methods
-
1. Age-based sizing:
Tracheostomy tube sizes are often recommended based on the child's age. Tracheostomy tube size for children 1 - 10 years of age (ID in mm) = (Age/4) + 3.5 to 4.
-
2. Weight-based sizing:
There isn't widely accepted formula specifically for calculating tracheostomy tube size in children based on weight. However, some clinicians use formulas developed for endotracheal tube (ETT) sizing as a rough guide: Weight-Based formula for paediatric ETT size. Khine et al.formula:
ETT size ( ID in mm) = (weight in kg/10) + 3.5 ( for cuffed tubes) or (weight in kg/10) + 4 ( for uncuffed tubes).
Keep in mind this formula is not specifically designed for tracheostomy tubes and tracheostomy tube sizing may vary depending on individual patient factors and clinical judgement. -
3. Measurement of tracheal diameter: In practice ,
tracheostomy tube size is often determined measuring the tracheal diameter using imaging studies or other methods such as bronchoscopy to help determine the appropriate tube size.
Clinical Judgment
-
1. Experience and expertise:
Clinicians should use their experience and expertise to select the most appropriate tracheostomy tube size for each child.
-
2. Individualized care:
Each child's needs should be individualized, and the tracheostomy tube size should be selected based on their specific requirements
Selecting the right tracheostomy tube size for a child is crucial to ensure effective ventilation, prevent complications, and promote optimal outcomes.
Complications
1. Intraoperative complications: Bleeding, damage to surrounding structures.
2. Early complications: Bleeding, infection, tube displacement.
3. Late complications: Tracheal stenosis, tracheoesophageal fistula.
Postoperative Care
1. Tracheostomy tube care: Regular cleaning and suctioning.
2. Humidification: Providing humidified air to prevent drying of the airway.
Management of Tracheo-Cutaneous Fistula
1. Surgical closure: Surgical closure of the fistula.
2. Conservative management: Conservative management may be attempted in some cases.
Postoperative Care
1. Regular tube changes: Regular changing of the tracheostomy tube.
2. Tracheostomy tube care: Regular cleaning and suctioning.
Decannulation
-
1. Assessment:
Assessment of the patient's ability to breathe without the tracheostomy tube.
-
2. Step-by-step protocol:
A step-by-step protocol for decannulation may vary depending on the institution and patient population.
The British and American methods for decannulation may have some differences, but the general principles involve assessing the patient’s ability to breathe without the tracheostomy tube and gradually weaning them off the tube.
Here’s a step-by-step approach to decannulation of a tracheostomy tube:
Pre-Decannulation Assessment:
-
1. Evaluate the patient's respiratory status:
Assess the patient's ability to breathe without the tracheostomy tube.
-
2. Check for adequate airway patency:
Ensure that the patient's upper airway is patent by indirect laryngoscopy, flexible nasolaryngoscopy, soft tissue X-ray of the neck, CT scan of neck and chest etc.
-
3. Assess the patient's ability to cough and clear secretions:
Evaluate the patient's ability to cough and clear secretions effectively.
Decannulation Protocol
-
1. Capping trial:
Cap the tracheostomy tube or cover with gauze to assess the patient's ability to breathe through the upper airway. In some cases the tracheostomy tube may need to be downsized before capping trial, especially in children.
-
2. Monitoring:
Closely monitor the patient's vital signs, oxygen saturation, and respiratory status.
-
3. Gradual weaning:
Gradually wean the patient off the tracheostomy tube, starting with capping trials and progressing to tube removal.
Post-Decannulation Care
-
1. Wound care:
Provide wound care and dressing to the tracheostomy site.
-
2. Monitoring:
Continue to monitor the patient's respiratory status and vital signs for about 24 hours, post tracheostomy tube removal, for inpatient, before discharge.
-
3. Follow-up:
Schedule follow-up appointments to assess the patient's airway and respiratory status.
Decannulation in Special Populations
-
1. Pediatric patients:
Decannulation in pediatric patients requires careful consideration and close monitoring. Tube may need to be downsized before capping.
-
2. Patients with complex airway anatomy:
Patients with complex airway anatomy may require specialized care and management.
The specific steps and protocol for decannulation may vary depending on the institution, patient population, and individual patient needs
Office-Based Decannulation
Office-based decannulation may be performed in selected patients with stable airways and minimal risk of complications. However, the decision to perform decannulation in an office setting should be made on a case-by-case basis, considering the patient's individual needs and risk factors.
Share Post On:
Recent Posts
-
Functional Endoscopic Sinus Surgery (FESS)
-
Tracheostomy
-
Clinical Voice Test (CVT) for Hearing Loss
-
Acute Epiglottitis And Approach To Management
-
Synoptic Overview Of Nasopharyngeal Carcinoma
-
Prioritizing Support For People With Disabilities Over Unhealthy Competitions That Marginalise The Downtrodden
-
Otitic Barotrauma
-
Titbits of Informed Consent Process for a Medical or Surgical Procedure
-
Comprehensive Overview of Mpox (Monkeypox)
-
Overview Of Corrosive Ingestion - Acid & Alkalis, and Management Approach
-
Ethical Conundrum
-
Comprehensive Overview of Laryngeal Papillomatosis and HPV Virus
-
All You Need To *Know About Gardasil*
-
Preauricular Sinus
-
Laryngomalacia - comprehensive overview
-
Flexible Laryngoscopy features of Laryngomalacia
-
Case Report of a Rare Cause of Upper Airway Obstruction In Adults
-
Usefulness of The Neck Soft Tissues X-Ray
-
Paranasal Sinuses Radiology
-
Swallow Function Test
-
Radiotherapy and Chemotherapy In Head And Neck Cancers
-
Myringoplasty
-
Overview of Chronic Suppurative Otitis Media (CSOM)
-
Overview Of Otitis Externa
-
What You Need To Know About Red Meat And Cancer
-
All You Need To Know About Cawthorne-Cooksey Vestibular Rehabilitation Exercises
-
Hoarseness Of Voice - Comprehensive Overview
-
Epleys Manoeuvre
-
Allergic rhinitis (AR)
-
The Discharging Ear In Children And Approach To Its Managements
-
All You Need To Know About Tinnitus
-
How is skin Prick Test Done for All
-
Orbital complications of rhinosinusitis
-
Sudden sensorineural hearing loss
-
Asymmetric sensorineural hearing loss (ASNHL)
-
What is rhinosinusitis?
-
Halitosis (Bad Breath) And Approach To Management
-
All You Need To Know About Sinus Rinse
Categories
Get in Touch
Read doctor-produced health and medical information written for you to make informed decisions about your health concerns.