Overview Of Otitis Externa
Overview
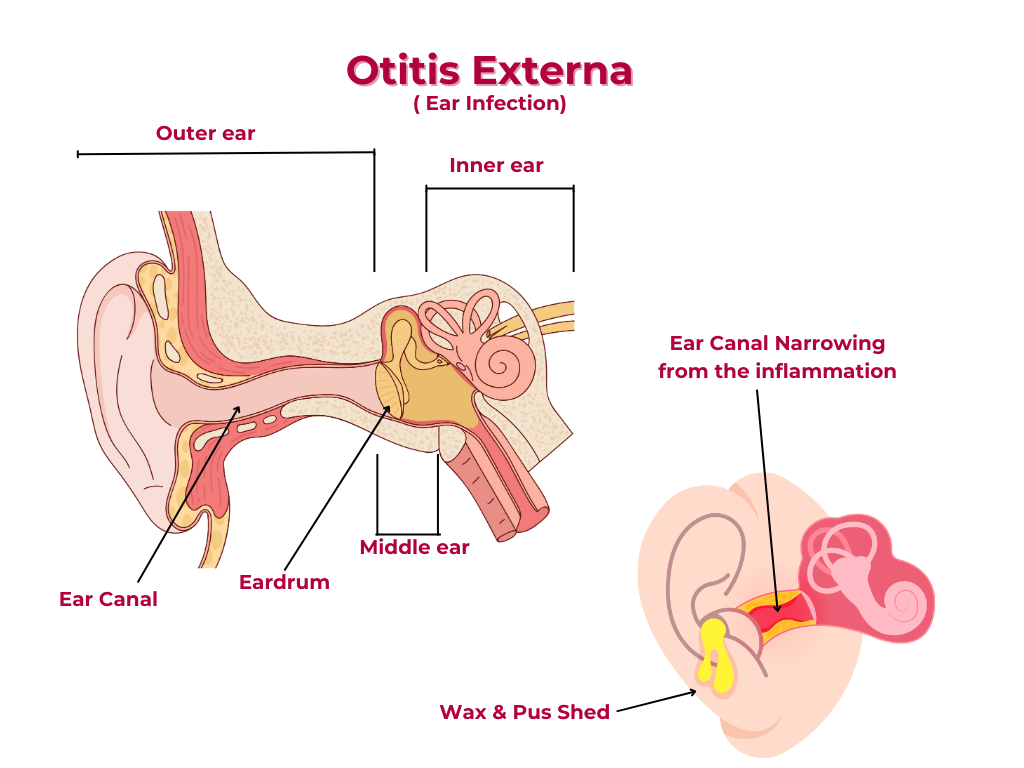
Otitis externa (OE) is an inflammatory condition of the external auditory canal (EAC), which can be caused by infection, allergy, or irritation.
Epidemiology
1. Prevalence: OE affects approximately 1-3% of the general population.
2. Age: OE can occur at any age, but it's more common in children and young adults.
3. Sex: Both males and females are equally affected.
Classification
What are the different types of Otitis Externa?
The different types of otitis externa include the following:
1. Acute otitis externa: Sudden onset of symptoms, typically lasting less than 3 weeks.
2. Chronic otitis externa: Persistent symptoms lasting more than 3 weeks.
3. Malignant otitis externa: A severe, necrotizing infection, typically occurring in immunocompromised individuals.
What are the degrees of Otitis Externa?
The degrees are:
1. Mild: Symptoms are mild, and the EAC is only slightly inflamed.
2. Moderate: Symptoms are more pronounced, and the EAC is moderately inflamed.
3. Severe: Symptoms are severe, and the EAC is severely inflamed.
Pathophysiology
1. Bacterial infection: Staphylococcus aureus, Pseudomonas aeruginosa, and other bacteria can cause OE.
2. Fungal infection: Fungi like Aspergillus and Candida can cause OE.
3. Allergic reaction: Allergies to ear drops, jewelry, or other substances can cause OE.
4. Irritation: Trauma, foreign bodies, or chemical exposure can cause OE.
Symptoms and signs
1. Ear pain: Pain or discomfort in the ear, which can radiate to the face or temple.
2. Itching: Itching or tickling sensation in the ear.
3. Discharge: Yellow or greenish discharge from the ear.
4. Hearing loss: Temporary hearing loss or a feeling of fullness in the ear.
5. Fever: Fever or malaise in severe cases.
Investigations
1. Otoscopic examination: Visual examination of the ear canal and eardrum.
2. Microbiological examination: Culture or sensitivity testing of ear discharge.
3. Imaging studies: CT or MRI scans to rule out complications or underlying conditions.
Complications
1. Cellulitis: Spread of infection to surrounding tissues.
2. Abscess formation: Collection of pus in the EAC or surrounding tissues
3. Mastoiditis: Infection of the mastoid bone.
4. Hearing loss: Permanent hearing loss or tinnitus.
Management and Treatment
This is a comprehensive overview, and treatment should always be individualized and guided by a healthcare professional.
1. Topical antibiotics: Ear drops or ointments containing antibiotics or antifungals.
2. Pain management: Analgesics or anti-inflammatory medications to manage pain and inflammation.
3. Cleaning and debridement: Gentle cleaning and removal of debris or discharge from the EAC.
4. Avoidance of irritants: Avoiding exposure to allergens, irritants, or trauma.
NOTE ON MALIGNANT OTITIS EXTERNA!!!
MALIGNANT OTITIS EXTERNA:
Malignant otitis externa (MOE) is a severe, potentially life-threatening infection of the external auditory canal and surrounding tissues.
Here's an overview of its pathophysiology:
Etiology
1. Pseudomonas aeruginosa: The primary causative agent, responsible for 90% of MOE cases.
2. Other bacteria: Staphylococcus aureus, Proteus, and Klebsiella can also contribute to MOE.
3. Fungal infections: Aspergillus and Candida can cause MOE, especially in immunocompromised patients.
Pathogenesis
-
1. Colonization
Pseudomonas aeruginosa colonizes the external auditory canal, often in patients with compromised immunity or pre-existing conditions.
-
2. Infection
The bacteria invade the canal's epithelial layer, causing inflammation and tissue damage.
-
3. Necrosis
The infection progresses, leading to necrosis of the canal's cartilaginous and bony structures.
-
4. Spread
The infection can spread to surrounding tissues, including the temporal bone, skull base, and cranial nerve
Risk Factors
1. Immunocompromised state: Diabetes, HIV/AIDS, chemotherapy, and immunosuppressive therapy increase the risk of MOE.
2. Age: Elderly patients are more susceptible due to decreased immunity and comorbidities.
3. Trauma: Trauma to the ear or head can increase the risk of MOE.
4. Pre-existing conditions: Conditions like otitis externa, eczema, or psoriasis can predispose individuals to MOE.
Clinical Manifestations
1. Severe otalgia: Pain is often intense and unresponsive to analgesics.
2. Otorrhea: Purulent discharge from the ear
3. Fever: High fever, often accompanied by chills..
4. Hearing loss: Conductive or sensorineural hearing loss can occur.
5. Facial paralysis: Involvement of the facial nerve can lead to paralysis.
Complications
1. Temporal bone osteomyelitis: Infection can spread to the temporal bone.
2. Skull base osteomyelitis: Infection can spread to the skull base.
3. Cranial nerve involvement: Infection can affect nearby cranial nerves.
4. Meningitis: In rare cases, MOE can lead to meningitis.
Treatment
1. Antibiotics: Aggressive antibiotic therapy, often with antipseudomonal agents.
2. Surgical debridement: Removal of necrotic tissue and debris.
3. Pain management: Aggressive pain management to control severe otalgia.
4. Supportive care: Management of underlying conditions, such as diabetes, and provision of nutritional support.
Early recognition and treatment are crucial to prevent complications and improve outcomes in patients with malignant otitis externa.
Share Post On:
Recent Posts
-
Technique of Incision and Drainage of Septal Hematoma/Septal Abscess
-
Upper Aerodigestive Tract Foreign Body Impaction
-
Incision and Drainage of Hematoma Auris
-
Rigid Bronchoscopy for Retrieval of Foreign Bodies in Children
-
Foreign Body Impaction in the Larynx, Trachea, and Bronchi
-
Leadership Position is a Tool, not a Trophy
-
Carcinoma of the Oropharynx
-
Peritonsillar Abscess
-
Ethics of Doctor-Patient Relationship
-
Doctor-Patient Relationship Case Scenarios
-
Asymmetrical Tonsils and Approach to Evaluation and Management
-
Nasal Polyposis
-
Rigid Oesophagoscopy and Complication
-
Anatomy of Oesophagus
-
Stridor, Snoring, Stertor And Wheezing: How They Compare
-
Temporomandibular Joint (TMJ)
-
Otoacoustic Emissions
-
Tympanometry
-
Functional Endoscopic Sinus Surgery (FESS)
-
Tracheostomy
-
Clinical Voice Test (CVT) for Hearing Loss
-
Acute Epiglottitis And Approach To Management
-
Synoptic Overview Of Nasopharyngeal Carcinoma
-
Prioritizing Support For People With Disabilities Over Unhealthy Competitions That Marginalise The Downtrodden
-
Otitic Barotrauma
-
Titbits of Informed Consent Process for a Medical or Surgical Procedure
-
Comprehensive Overview of Mpox (Monkeypox)
-
Overview Of Corrosive Ingestion - Acid & Alkalis, and Management Approach
-
Ethical Conundrum
-
Comprehensive Overview of Laryngeal Papillomatosis and HPV Virus
Categories
Get in Touch
Read doctor-produced health and medical information written for you to make informed decisions about your health concerns.

